How to Get Rid of Man Boobs: Your Complete Guide to Gynecomastia Surgery

Dr. Delgado with a patient discussing his gynecomastia.
Dealing with enlarged male breasts affects millions of men worldwide, with studies showing that up to 65% of adolescent boys and 35% of adult men experience some degree of breast enlargement at some point in their lives. While this condition, medically known as gynecomastia, is far more common than most people realize, it can significantly impact self-confidence and mental health. Most often, gynecomastia isn’t a serious problem, but it can be tough to cope with the condition. Gynecomastia is associated with significant psychological distress, social stigma, and dysphoria, further emphasizing the importance of effectively addressing the condition.
If you’ve been struggling with man boobs and wondering how to get rid of them permanently, you’re in the right place. This comprehensive guide will guide you through everything you need to know about gynecomastia surgery, from understanding the underlying causes to choosing the right surgeon and managing your recovery.
For many men, exercise and diet changes simply aren’t enough to address the underlying glandular breast tissue that characterizes true gynecomastia. When non-surgical treatments fall short, male breast reduction surgery offers a definitive solution with excellent long-term results and high patient satisfaction rates.
Key Takeaways
- Gynecomastia surgery is the most effective permanent solution for man boobs, with success rates over 95% when performed by qualified surgeons.
- Two main surgical techniques exist: liposuction for the removal of fatty tissue, excision for the removal of glandular tissue, and excess skin removal.
- Most patients return to work within 3 to 7 days and resume normal activities within 2 to 3 weeks after surgery.
- Non-surgical methods, such as exercise and diet, can help with pseudogynecomastia (fat-based), but cannot eliminate true glandular tissue.
- Surgery costs typically range from $8,000 to $10,000 and are rarely covered by insurance, as it’s considered a cosmetic procedure. However, this does not include anesthesia or surgical facility fee. The medication and tissue pathology is usually covered with health insurance.

A doctor explaining the characteristics and treatment for gynecomastia.
Introduction to Gynecomastia
Gynecomastia is a medical condition that causes the enlargement of breast tissue in males, affecting up to 65% of men at some point in their lives. The condition can affect one or both breasts, and the enlargement may be uneven (asymmetrical) or symmetrical. While often referred to as “man boobs” or “moobs,” it’s important to recognize that gynecomastia is a genuine health concern that can cause significant emotional distress and self-consciousness. Many men who develop enlarged breasts find the condition impacts their self-esteem and quality of life, prompting them to seek effective treatment options. Male breast reduction surgery is one of the most reliable solutions for those struggling with persistent breast enlargement. Various factors can trigger gynecomastia, including hormonal changes, certain medications, underlying health conditions, and certain medical conditions. Male breast reduction can be performed safely on both teenagers and adult men. Lower testosterone levels, often due to certain health conditions, can disrupt the hormonal balance and contribute to the development of gynecomastia. Identifying the underlying cause is essential for developing a personalized treatment plan, whether that involves surgery or other approaches. By understanding the nature of gynecomastia and the available treatments, men can take proactive steps to restore their confidence and achieve a more masculine chest contour.
Understanding Gynecomastia vs Pseudogynecomastia

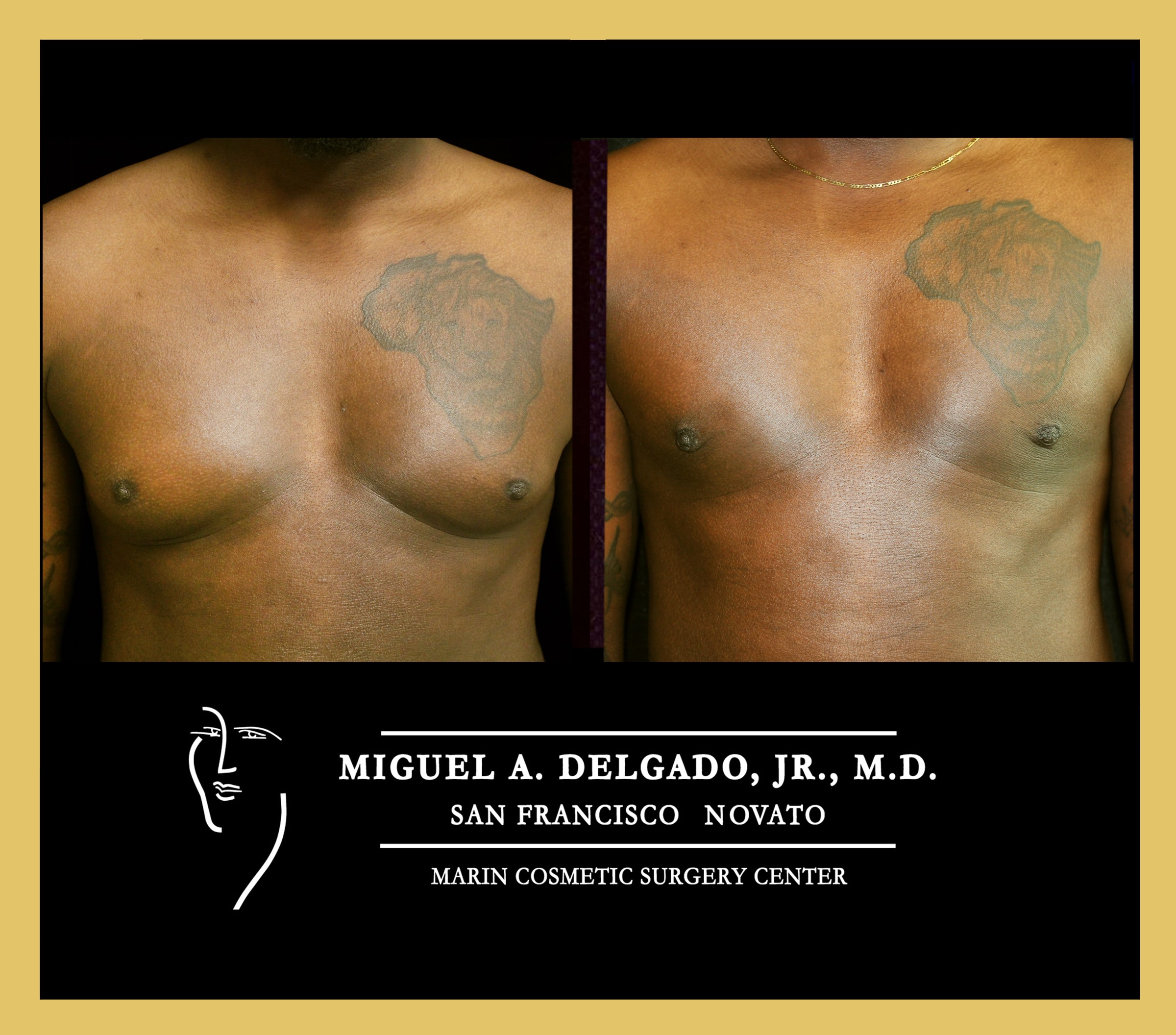
A patient of Dr. Delgado with excellent skin elasticity : Before and after photo of gynecomastia surgery
Before exploring surgical options, it’s crucial to understand what type of breast enlargement you’re dealing with. The term gynecomastia specifically refers to the enlargement of glandular breast tissue in males, while pseudogynecomastia describes enlarged male breasts caused primarily by excess fat tissue without significant glandular involvement.
True gynecomastia involves the proliferation of actual breast tissue behind the nipple area, creating a firm, sometimes tender mass that cannot be eliminated through diet and exercise alone. This glandular tissue develops due to hormonal imbalances, medications, medical conditions, or genetic factors that affect the levels of testosterone and estrogen in the body. Genetic conditions such as Klinefelter syndrome can also lead to gynecomastia by altering hormone ratios and increasing estrogen. Additionally, thyroid disease can disrupt hormonal balance and is linked to gynecomastia, further complicating the condition.
Pseudogynecomastia, on the other hand, results from excess body fat accumulation in the chest area and typically affects overweight men. Unlike true gynecomastia, pseudogynecomastia can often be improved if you lose weight and focus on targeted exercise. However, losing weight may not address true glandular tissue, so some men may still require surgical intervention for optimal results.
During a physical examination, healthcare providers can distinguish between these conditions by palpating the breast area. Gynecomastia typically presents as a firm, disc-like mass of glandular breast tissue directly beneath the nipple and areola, while pseudogynecomastia feels softer and more diffuse throughout the chest. Most occurrences of gynecomastia do not require diagnostic tests.
The hormonal causes of gynecomastia are complex and can involve several factors. Declining testosterone levels, increased estrogen production, certain medications including anabolic steroids, medical conditions affecting the liver or kidneys, and even tumors of the pituitary gland or adrenal glands can contribute to hormone changes that trigger excess glandular tissue growth.
Age-related statistics reveal interesting patterns in the prevalence of gynecomastia. While approximately 70% of adolescent boys experience some degree of breast enlargement during puberty, this often resolves naturally as hormone levels stabilize. Even male babies can develop gynecomastia due to exposure to maternal hormones, but this usually resolves on its own. However, 35% of adult men continue to struggle with enlarged breasts, with peak incidence occurring between 50 and 69, when testosterone levels naturally decline.
Non-surgical and surgical options are available for treating gynecomastia. However, other treatments, such as medication or addressing underlying causes, may be considered case-by-case.
Causes of Enlarged Breasts in Men

Young man with enlarged breast due to medication induced gynecomastia.
Enlarged breasts in men, medically known as gynecomastia, can develop for various reasons. One of the most common causes is hormonal imbalance—specifically, an increase in estrogen levels or a decrease in testosterone levels. Testosterone usually prevents breast tissue from expanding in males. Estrogen stimulates the growth of breast tissue, and when its effects outweigh testosterone, men may notice breast enlargement. The use of anabolic steroids, certain medications (such as antidepressants, antibiotics, or drugs for heart conditions), and some medical conditions can also disrupt hormone levels and contribute to gynecomastia. Conditions affecting the liver, kidneys, or endocrine system may play a role, as can tumors that alter hormone production. In some cases, gynecomastia is a symptom of an underlying medical condition that requires further investigation. Because the causes of gynecomastia are so varied, it’s important to consult a healthcare provider to determine the underlying cause and develop an effective treatment plan tailored to each individual’s needs.
Understanding Breast Tissue

Diagram of normal male breast tissue and one with gynecomastia.
Male breast tissue is composed of both glandular tissue and fat, and understanding this composition is crucial for addressing gynecomastia. In cases of true gynecomastia, there is an overgrowth of glandular tissue, which is particularly sensitive to hormone levels changes—especially the balance between estrogen and testosterone. This excess glandular tissue can cause the breasts to feel firm or rubbery, and sometimes lead to symptoms such as breast tenderness, nipple discharge, or other changes in the breast area. These symptoms can be distressing and may prompt men to seek medical advice. Male breast reduction surgery targets this glandular tissue, removing the excess to restore a flatter, more masculine chest. By understanding how breast tissue responds to hormonal changes and other factors, patients and their doctors can select the most effective treatments — whether surgical or non-surgical — to address both the physical and emotional aspects of gynecomastia.
When Non-Surgical Methods Fall Short
Many men spend years attempting to address their enlarged male breasts through diet, exercise, and lifestyle modifications, before considering surgical options. While these approaches can be effective for pseudogynecomastia caused by excess fat, they have significant limitations when dealing with true glandular tissue. Weight loss achieved through cardiovascular exercise and dietary changes can help reduce excess body fat and diminish the appearance of enlarged male breasts in cases of pseudogynecomastia.
Cardiovascular exercise and chest-focused workouts can certainly help build muscle mass in the pectoral muscles and reduce body fat, but they cannot eliminate the glandular breast tissue that characterizes true gynecomastia. In fact, some men find that building chest muscles actually makes their breast enlargement more prominent by pushing the glandular tissue forward.
Compression garments and specific clothing modifications can provide temporary cosmetic improvement by flattening the chest appearance. However, these solutions don’t address the underlying tissue and can be uncomfortable or impractical for daily wear, especially in warm weather or during physical activities.
Several medication options exist for treating gynecomastia, including selective estrogen receptor modulators like tamoxifen and aromatase inhibitors that block estrogen production. However, these medical treatments typically show success rates of only 20-40% and are most effective when started early in the course of the condition. They’re also associated with potential side effects and require ongoing monitoring by healthcare providers.
Most medical experts recommend considering surgical options when gynecomastia has been present for more than two years without improvement, as the likelihood of spontaneous resolution decreases significantly after this timeframe. For men whose condition persists beyond this point or causes significant psychological distress, male breast reduction surgery offers the most reliable path to permanent improvement.
The decision to pursue gynecomastia surgery often comes after men have exhausted other treatment options and recognize that non-surgical approaches cannot address their specific type of breast tissue enlargement. Understanding these limitations helps set realistic expectations and guides patients toward the most appropriate treatment for their individual situation.

Images depicting the stages of gynecomastia, from Grade 1 with puffy nipples to Grade 4 with excess skin.
Types of Gynecomastia Surgery for Excess Breast Tissue
Male breast reduction surgery encompasses several techniques, each designed to address specific types of tissue excess and varying degrees of enlargement. For example, liposuction is often performed through small incisions, allowing the surgeon to remove excess fat tissue with minimal scarring. This minimally invasive approach is particularly effective when the enlarged breast tissue is primarily composed of fat rather than glandular tissue. The choice of surgical procedure depends on the grade of gynecomastia, the composition of excess tissue (fat versus glandular), and the amount of excess skin present.
Plastic surgeons typically use a grading system to classify the severity of gynecomastia and guide surgical planning. Grade I involves small enlargement without excess skin, Grade II includes moderate enlargement with (IIb) or without (IIa) excess skin, and Grade III presents marked enlargement with significant excess skin requiring more extensive surgical intervention.
Liposuction for Gynecomastia
Liposuction techniques have evolved significantly, offering excellent options for removing excess fat tissue while minimizing scarring. VASER liposuction technology uses ultrasonic energy to selectively target fat cells while preserving surrounding tissues, resulting in smoother contours and reduced recovery time.
Power-assisted liposuction (PAL) represents another advanced technique that uses mechanical vibration to break up fat deposits more efficiently. This approach allows surgeons to remove larger volumes of tissue through smaller incisions, while maintaining precise control over the contouring process.
The liposuction procedure typically begins with tumescent fluid injection, a solution containing local anesthetic and epinephrine that helps reduce bleeding and post-operative pain. Surgeons then insert small cannulas through tiny incisions, usually measuring just 3-4mm, strategically placed to minimize visible scarring.
Expected fat removal volumes vary based on individual anatomy, but typically range from 200-800ml per side. The minimal scarring associated with liposuction-only approaches makes this technique attractive for men with primarily fatty tissue excess and good skin elasticity.
Surgical Excision Techniques

Patient with grade 3 gynecomastia after gynecomastia surgery with skin excision at 3 months.
When significant glandular tissue or excess skin is present, surgical excision becomes necessary to achieve optimal results. The most common approach involves periareolar incisions placed along the natural border between the areola and surrounding skin, which heal with minimal visible scarring.
Glandular tissue removal typically involves excising 50-200g of tissue per side, depending on the severity of enlargement. Surgeons must carefully preserve adequate tissue to maintain natural chest contours, while removing enough material to eliminate the feminine appearance.
For cases involving enlarged or malpositioned nipple-areola complexes, repositioning procedures can restore more masculine proportions. This may involve reducing areola size, lifting the nipple position, or both, depending on individual anatomy and aesthetic goals.
More extensive skin excision patterns become necessary in severe cases where significant skin redundancy exists. These procedures may involve larger incisions, but are essential for achieving tight, masculine chest contours in patients with Grade III gynecomastia.
Advanced tissue preservation techniques enable surgeons to achieve natural-looking results while removing sufficient tissue to effectively treat the condition. This requires careful attention to maintaining the appropriate thickness of remaining tissue and preserving the blood supply to the nipple-areola complex.
Pre-Surgery Preparation
Preparing for gynecomastia surgery, or male breast reduction surgery, involves several important steps to ensure the best possible outcome. The surgical procedure is designed to remove excess breast tissue—both glandular tissue and fat—to create a more masculine chest shape. Before surgery, patients should provide a complete medical history and undergo a thorough physical examination to identify any underlying medical conditions that could affect the procedure or recovery. It’s essential to stop taking certain medications, such as blood thinners, and to avoid smoking and alcohol in the weeks leading up to surgery, as these can interfere with healing. The surgeon will explain the details of the surgical procedure, including the location of incisions and what to expect during recovery. Patients should also be aware of potential risks and complications, such as infection, scarring, or changes in nipple sensation, and discuss any concerns with their surgeon. With careful preparation and clear communication, male breast reduction surgery can be a highly effective treatment for gynecomastia, helping men regain confidence and comfort in their appearance.
The Complete Surgical Process
Understanding the entire surgical journey helps patients prepare mentally and physically for their male breast reduction surgery. The process begins weeks before the actual procedure, and continues through several months of recovery and follow-up care.
The initial consultation includes a comprehensive physical examination, a review of your medical history, and a discussion of your treatment goals and expectations. Surgeons evaluate the type and extent of breast tissue enlargement, assess the quality and elasticity of the skin, and determine the most appropriate surgical approach for each individual case.
Preoperative testing requirements may include a complete blood count (CBC), comprehensive metabolic panel, hormone level assessments, and occasionally mammography or ultrasound imaging to rule out underlying pathology. Screening for male breast cancer is an important part of the evaluation process to rule out malignancy before surgery. These tests help ensure patient safety and identify any medical conditions that might affect surgical outcomes.
Medication adjustments begin approximately two weeks before surgery, with patients typically required to stop blood-thinning medications, anti-inflammatory drugs, and certain supplements that might increase bleeding risk. Patients must also address any underlying medical conditions and optimize their general health status.
Smoking cessation is one of the most critical pre-operative requirements, with surgeons typically requiring patients to stop all tobacco and nicotine use for at least four weeks before and after surgery. Nicotine significantly impairs wound healing and increases the risk of complications, making this requirement non-negotiable for most surgeons.
During Surgery
A patient after minimal invasive gynecomastia surgery.
The day of surgery typically begins with arrival at the surgical facility 1 to 2 hours before the scheduled procedure time. Patients undergo final pre-operative assessments, meet with the anesthesia team, and have surgical sites marked while standing upright to ensure optimal symmetry.
Anesthesia options include local anesthesia with intravenous sedation for less extensive procedures, or general anesthesia for more complex cases involving significant tissue removal or skin excision. The choice depends on the planned surgical technique, patient preferences, and surgeon recommendations.
Surgical duration varies considerably depending on the complexity of the case, ranging from 1-3 hours for most procedures. Simple liposuction-only cases may require just 60-90 minutes, while combined approaches with excision and skin removal can take 2-3 hours to complete safely.
Throughout the surgical procedure, careful attention is paid to achieving symmetric results, maintaining natural chest contours, and preserving blood supply to the nipple-areola complex. Surgeons use various measurement techniques and frequent assessment to ensure optimal outcomes.
Immediate post-operative care includes the application of compression dressings or specialized garments, administration of pain medication, and assessment of initial results. Most patients are discharged the same day as their outpatient procedure, provided they meet specific recovery criteria and have the supervision of a responsible adult. Surgery for male breast reduction is usually an outpatient procedure, allowing patients to go home the same day.
Recovery Timeline and Expectations
The first 48 hours after surgery represent the most critical period for pain management and initial healing. Most patients experience moderate discomfort that responds well to prescribed pain medications, with pain levels typically rating 4-6 out of 10 during this initial period. Patients may also experience soreness in the chest area for several days after surgery, but this typically improves with medication and time. It is normal to feel sore after gynecomastia surgery, and this soreness usually subsides within a few days to weeks as part of the normal healing process. Moderate pain, swelling, and bruising are common after surgery. Recovery after gynecomastia surgery typically involves wearing a supportive garment to reduce swelling. They gradually subside over the following weeks, marking steady progress in recovery.
Week one involves continuously wearing compression garments, limiting arm movement to avoid stress on healing incisions, and focusing on rest and gentle movement. Patients can usually shower after 24-48 hours, but must keep incision sites dry and follow specific wound care instructions.
Weeks 2-3 mark the beginning of a gradual return to normal activities, with most patients able to return to desk work and light activities. Compression garment wear continues, but patients typically experience significant improvement in comfort and mobility during this period. Recovery typically lasts between four and six weeks, with final results fully visible over several months as swelling subsides and tissues settle into their new position.
The 4-6 week timeframe allows for resumption of exercise and heavy lifting activities, though surgeons provide specific guidelines based on individual healing progress. Most swelling subsides during this period, revealing more accurate representations of final results.
Final results become fully apparent 3-6 months after surgery, as all swelling resolves completely and tissues settle into their new position. During this time, patients can assess the final outcome and determine if minor revisions might be beneficial.
Choosing the Right Surgeon

Dr. Delgado, a board certified plastic surgeon and gynecomastia specialist.
Selecting a qualified surgeon is one of the most important decisions in the gynecomastia surgery process. The expertise and experience of your chosen surgeon directly impact both the safety of your procedure and the quality of your results.
Board certification in plastic surgery or cosmetic surgery provides the foundation for a surgeon’s qualification. These certifications require extensive training, ongoing education, and demonstrated competency in surgical techniques specific to aesthetic and reconstructive procedures.
Specific experience with male breast reduction procedures is crucial, as gynecomastia surgery requires specialized knowledge of male chest anatomy and aesthetic ideals. Look for surgeons who perform at least 50+ gynecomastia procedures annually, as this volume ensures ongoing refinement of technique and familiarity with various case complexities.
A comprehensive before-and-after photo portfolio allows potential patients to assess the surgeon’s aesthetic judgment and technical skill. Review multiple cases similar to your own condition, paying attention to symmetry, natural-looking results, and the quality of scar placement.
Hospital privileges and surgery in accredited facilities provide additional assurance of safety. Surgeons with hospital privileges have undergone credentialing processes that verify their training and competency, while accredited surgical facilities meet strict safety and equipment standards.
Patient testimonials and online reviews provide valuable insights into the patient experience, including the quality of communication, staff professionalism, and satisfaction with the results. Look for patterns in feedback and pay attention to how surgeons respond to negative reviews or concerns.
During consultation appointments, assess the surgeon’s communication style, willingness to answer questions thoroughly, and ability to explain procedures in understandable terms. A qualified surgeon should provide realistic expectations, discuss potential risks openly and honestly, and demonstrate genuine interest in achieving your specific goals.
Costs and Insurance Considerations
Understanding the financial aspects of gynecomastia surgery enables patients to plan effectively and make informed decisions about their treatment options. Costs vary significantly based on geographic location, surgeon experience, facility type, and complexity of the required surgical procedure.
Average surgery costs typically break down into several components: surgeon fees ranging from $8,000 to $10,000, surgical facility fees of $500 to $1,500, and anesthesia costs of $1,000 to $1,300. Additional expenses may include lab test if needed, pathology, post-operative medications, and compression garments. Medications and tissue pathology is often covered by health insurance.
Geographic cost variations across major U.S. cities can be substantial, with procedures in metropolitan areas like New York, Los Angeles, and Miami typically cost more than those in smaller cities or rural areas. However, patients should prioritize surgeon qualification and experience over cost considerations when making their selection.
Insurance coverage for gynecomastia surgery remains limited, as most insurance companies classify the procedure as cosmetic rather than medically necessary. Coverage criteria, when they exist, typically require documentation of significant psychological distress, failed medical therapy, and sometimes evidence of breast cancer risk factors.
To qualify for potential insurance coverage, patients typically require extensive documentation, including medical history records, photographs, psychological evaluations, and letters from multiple healthcare providers, that support the medical necessity of the surgical treatment. Even with this documentation, approval rates remain low.
Financing options and payment plans have become increasingly available through specialized medical financing companies and some surgical practices. These options enable patients to spread the cost of surgery over 12-60 months, with varying interest rates and qualification requirements.
When comparing costs with non-surgical alternatives, surgery often proves more cost-effective over time. While the initial investment is significant, the permanent nature of surgical results eliminates ongoing expenses, such as compression garments, medications, or repeated non-surgical treatments that may only provide temporary improvement.
Risks and Complications
Like any surgical procedure, gynecomastia surgery carries certain risks and potential complications that patients must understand before making treatment decisions. While serious complications are rare when qualified surgeons perform surgery in appropriate facilities, being informed about possible issues helps patients make educated choices and recognize signs that require medical attention. Complications can include excessive bleeding, infection, and visible scarring, which may require realistic expectations based on the patient’s specific situation.
Common temporary side effects affect most patients to some extent, and typically resolve within 2-6 months. These include swelling, bruising, temporary numbness of the chest and nipple area, and mild asymmetry during the healing process. Most patients find these effects manageable and accept them as normal parts of the recovery process.
More significant but still relatively common issues include seroma formation (fluid accumulation), minor wound healing problems, and temporary changes in nipple sensation. These complications occur in approximately 5-15% of cases, but usually resolve with appropriate treatment and don’t affect final results.
Rare but serious complications require immediate medical attention and can impact both safety and outcomes. Infection occurs in less than 1% of cases when proper surgical protocols are followed, while hematoma (blood accumulation) affects 2-3% of patients and may require drainage procedures.
Asymmetry requiring revision surgery affects 5-10% of patients. However, minor asymmetries are common and often improve over time. Factors contributing to asymmetry include differences in tissue composition between the sides, variations in healing, and occasionally technical factors during surgery.
Scarring expectations vary based on surgical technique, with periareolar incisions typically healing well with minimal visibility. However, some patients may develop thicker scars or keloid formation, particularly those with genetic predispositions to abnormal scar formation.
Signs requiring immediate medical attention include excessive bleeding, signs of infection (such as fever, increased redness, warmth, or drainage), severe or worsening pain, and any concerns about wound healing. Patients should have clear instructions on how to contact their surgeon and access emergency care if needed.
According to recent studies, long-term satisfaction rates exceed 95%, with most patients reporting significant improvements in self-confidence, body image, and quality of life. These high satisfaction rates reflect both the effectiveness of modern surgical techniques and appropriate patient selection by experienced surgeons.
Maintaining Long-Term Results
Achieving excellent results from gynecomastia surgery is only the beginning of the journey. Maintaining those results over the long term requires ongoing attention to lifestyle factors, medical monitoring, and general health maintenance.
Weight management plays a crucial role in preserving surgical outcomes, as significant weight gain can lead to the accumulation of new fat in the chest area. While the removed glandular tissue cannot regenerate, gaining more than 20 pounds above post-surgical weight may compromise the improved chest contour achieved through surgery.
Regular hormone monitoring and medical follow-ups help identify and address any underlying conditions that could contribute to breast tissue enlargement. Men with persistent hormonal imbalances, certain medical conditions, or those taking medications that affect hormone levels may require ongoing medical management to prevent recurrence.
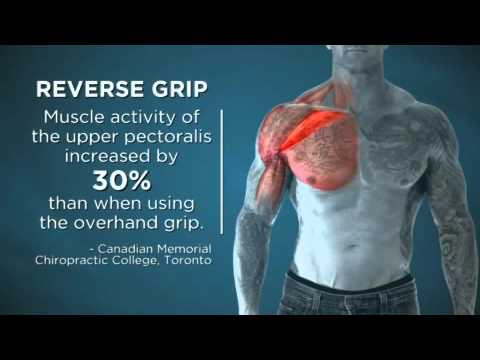
Exercise recommendations focus on maintaining overall fitness while building and preserving chest muscle mass. Regular strength training that targets the pectoral muscles helps maintain chest definition and enhances the masculine appearance achieved through surgery. However, patients should avoid overdeveloping their chest muscles, as this could create an unnatural appearance.
Medication avoidance becomes particularly important for men who have undergone gynecomastia surgery. Anabolic steroids, certain antidepressants, anti-anxiety medications, and some blood pressure medications can contribute to breast tissue enlargement. They should be avoided when possible, or used only under careful medical supervision.
Avoiding substances that can contribute to gynecomastia includes limiting alcohol consumption, avoiding marijuana use, and steering clear of anabolic steroids or other performance-enhancing substances. These substances can disrupt hormone balance and potentially contribute to the growth of new tissue.
Annual check-ups with your surgeon or primary care physician help monitor results and address any concerns early. During these appointments, healthcare providers can assess the chest contour, check for any signs of tissue regrowth, and discuss lifestyle factors that may affect long-term outcomes.
Patients should contact their surgeon if they notice significant changes in their chest appearance, the development of new lumps or masses, persistent pain or tenderness, or other concerning symptoms. Early intervention can often address minor issues before they become more significant problems.
Understanding that some natural aging changes will occur over time helps set realistic long-term expectations. While surgical results are generally permanent, factors such as skin aging, weight fluctuations, and natural tissue changes may cause minor alterations in chest appearance over time.
Ready to take the next step toward permanently getting rid of your man boobs? Don’t let gynecomastia continue to affect your self-confidence and quality of life. Contact Dr. Delgado’s office today at gynecomastia.org to schedule your consultation and explore your surgical options. With his extensive experience in male breast reduction surgery, Dr. Delgado can help you achieve the masculine chest contour you’ve been seeking.
Why chose Dr. Delgado for your surgery?
Dr. Miguel Delgado is a renowned expert in gynecomastia surgery with decades of experience specializing exclusively in male breast reduction. His deep understanding of the unique anatomical and psychological aspects of gynecomastia allows him to tailor surgical plans precisely to each patient’s needs. Dr. Delgado’s approach emphasizes natural-looking results that restore a masculine chest contour while minimizing visible scarring.
Patients consistently praise Dr. Delgado for his compassionate bedside manner and thorough consultations, where he ensures all questions are answered and realistic expectations are set. His commitment to patient education empowers men to make informed decisions about their treatment options.
Utilizing the latest surgical techniques, including advanced liposuction technologies and refined excision methods, Dr. Delgado achieves high success rates with minimal complications. His meticulous attention to detail during surgery helps preserve nipple sensation and symmetry, which are critical for patient satisfaction.
Dr. Delgado’s surgical center is equipped with state-of-the-art facilities, ensuring the highest standards of safety and comfort. He and his experienced team provide comprehensive preoperative and postoperative care, guiding patients through every step of their recovery to optimize healing and outcomes.
Whether you are a teenager experiencing persistent adolescent gynecomastia or an adult seeking a permanent solution to enlarged male breast tissue, Dr. Delgado’s expertise offers the confidence and results you deserve. His personalized approach ensures that each patient achieves a chest contour that enhances self-esteem and quality of life.
Call Today!
Dr. Delgado welcomes you for a complimentary consultation or call 415-898-4161.
Conclusion
Gynecomastia, or enlarged male breast tissue, is a condition that affects more than half of all men at some point in their lives. It results from hormone changes—specifically, an imbalance between estrogen and testosterone—that lead to excess breast tissue. This can be triggered by natural life stages, certain medications, underlying health conditions, or lifestyle factors. Symptoms such as swollen breast tissue, breast tenderness, and even nipple discharge can cause significant discomfort and concern.
For many people with gynecomastia, the impact goes beyond physical symptoms. The presence of excess glandular tissue can make men feel embarrassed, self-conscious, and anxious about their appearance, often affecting their self-esteem and mental health. Addressing gynecomastia is not just about improving the look of the chest—it’s about restoring confidence and quality of life.
Male breast reduction surgery, also known as gynecomastia surgery, is a highly effective treatment for those struggling with persistent or severe cases of enlarged male breast tissue. This surgical procedure removes excess glandular tissue and fat, helping create a flatter, more masculine chest contour. With the expertise of a qualified plastic surgeon, men can achieve lasting results and regain their self-assurance.
While surgery is the most effective treatment for significant or stubborn cases, other treatments may be appropriate for milder forms of gynecomastia. These can include hormone therapy, lifestyle changes, and addressing the underlying cause—such as switching certain medications or managing health conditions that contribute to hormone imbalance. Losing weight and building muscle, especially in the chest area, can also help reduce the appearance of excess breast tissue in some cases.
Preventing gynecomastia involves maintaining a healthy lifestyle, being mindful of medications and substances that can affect hormone levels, and seeking prompt medical attention for any new symptoms. Early intervention can help manage symptoms and prevent progression to more severe cases that may require surgery.
Ultimately, gynecomastia is a common and treatable condition. By understanding the causes, recognizing the symptoms, and exploring the full range of treatment options—including male breast reduction surgery—men can take control of their health and well-being. Consulting with a qualified healthcare professional is the first step toward finding the most effective treatment and achieving a more confident, masculine body image.
FAQ’s
Will gynecomastia surgery leave visible scars? Most scars fade significantly within 12-18 months and become barely noticeable, especially with periareolar incisions that follow the natural border of the areola. The final scar appearance depends on factors such as skin type, healing ability, and post-operative care. However, experienced surgeons employ techniques designed to minimize scarring.
Can gynecomastia return after surgery? Recurrence is rare (less than 5%) when glandular tissue is completely removed, though significant weight gain or hormonal imbalances can cause new fat accumulation. The removed glandular breast tissue cannot regenerate, making surgical results generally permanent when underlying causes are controlled.
What’s the minimum age for gynecomastia surgery? Most surgeons recommend waiting until at least 18 years old, or when breast development has been stable for 2+ years, as adolescent gynecomastia often resolves naturally. Surgery in younger patients is only considered in severe cases, causing significant psychological distress after thorough evaluation.
How long will it take before I can see the final results? Initial improvement is immediate, but the final results become apparent after 3-6 months, once all swelling subsides and the tissues have settled into their new position. Some minor improvements in contour and scar appearance may continue for up to 12-18 months after surgery.
Is the surgery painful? Most patients rate their pain as 4-6/10 for the first few days, which is easily managed with prescribed pain medication, and discomfort typically resolves within one week. Modern pain management techniques and surgical approaches have significantly reduced post-operative discomfort compared to older methods. Some men experience temporary sensation loss in the treated areas after surgery, which usually returns over time.